Tendonitis vs. Tendinosis…What’s the Difference and How are They Treated?

“Doc, I used to get tendonitis in my knee, but ibuprofen would take care of it in a few days.
Now, no matter what I do, it hurts.
What’s frustrating is that I took a couple of months off, did some physical therapy, and it was feeling good, but as soon as I started ramping back up, the pain returned.
Why isn’t my tendonitis going away this time?”
Unfortunately, I hear complaints like this often. The short answer, it is not tendonitis; it is likely tendinosis. Their difference requires a longer explanation, but I think it is essential to understand if you want to avoid chronic tendon pain and possible surgery.
My name is Dr. Ryan Sieg. I am an orthopedic surgeon at the Darnall Medical Center and the Medical Director of Sonex Orthopedics in Austin. You may think I spend most of my time seeing patients for blown-out joints and fractures, but in reality, most of my patients have chronic overuse injuries like tendonitis and tendinosis.
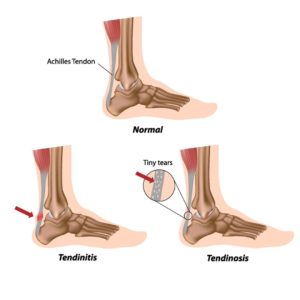
I will not bore you with a bunch of medical terms, but it is probably best to start with the meaning of “-itis” and “-osis.” “-Itis” indicates an inflammatory process while “-osis” indicates a degenerative process. Tendonitis is an inflamed tendon, while tendinosis is a degenerated tendon. I do not have to tell you which one is worse.
When you overload a tendon with repetitive motions or too much tension, tears form and you feel pain. Tears range from micro-tears that you may barely notice to complete ruptures that you will definitely notice. Let us focus on the micro-tears. With micro-tears, you will likely have some pain, but it is often one of those “sore in the morning” types of injuries. Your body initiates an inflammatory response when the micro-tear occurs.
Courtesy of Sonex Orthopedics.
Now, I know what you are thinking; inflammation is terrible. Actually, an acute inflammatory response is good because that is your body trying to heal the injury. Blood rushes to the area, which causes swelling, and your body begins repairing the damage. Full recovery from a minor injury typically takes anywhere from a few days to a few weeks, depending on the severity. Still, the tendon fully heals most of the time with the proper rest and treatment.
Being honest, most of us do not give a “tweaked” tendon enough time to heal. We may take a couple of days off, pop some ibuprofen, and slap a brace on before returning to activities because “it doesn’t hurt THAT bad.” The continued stress and possibly additional trauma to the tendon causes a prolonged inflammatory response, or tendonitis.
During this prolonged response that can last weeks or months, your body cannot properly repair the injury. Instead of fixing the micro-tear with healthy tendon tissue in uniform strands, you get disorganized collagen bands, blood vessels, and nerves. This tissue is more like scar tissue and provides no tensile strength.
If it is just a micro-tear, what is the big deal? The problem is that this cycle repeats over the years. Those small scar tissue pockets start adding up to a large area of scar tissue that your body essentially gives up trying to heal. Bam, it is now tendinosis.
Tendinosis, the degeneration of a tendon, consists of changes in tendon structure and composition, and no inflammatory response. Instead of white organized fibers, your tendon has disorganized fibers and is thicker with a brownish appearance. What is even worse is that your tendon is now weaker and more susceptible to rupture.
Remember those disorganized blood vessels I mentioned earlier? Well, tendons receive poor blood flow. The disorganized blood vessels further decrease blood flow to the injured area and impede healing.
The good news is that tendinosis usually responds to non-surgical treatments such as physical therapy, bracing, and rest. Recovery can take four to six months, but severe cases sometimes require surgery (or, High-energy Extracorporeal Shockwave Therapy) to debride the tendon.

Courtesy of Sonex Orthopedics.
A tendon debridement is when an orthopedic surgeon exposes the tendon and literally scrapes away the scar tissue. After the short surgery, your joint is typically immobilized for six to eight weeks to allow your tendon to heal properly. The total recovery time is four to six months. The results are generally good, but some patients are unable to return to sports activities.
High-energy Extracorporeal Shockwave Therapy is a non-invasive alternative to debridement surgery and the treatment we specialize in at Sonex Orthopedics. The treatment uses powerful acoustic shockwaves that are focused on the damaged portion of the tendon. The shockwave’s energy breaks apart scar tissue, causes new blood vessels to form, and stimulates the body’s healing processes to repair the damaged tendon. You can return to routine activities right after your treatment but will have to avoid high-impact activities for about 30 days as the tendon heals. I am a surgeon, and most people think surgeons want to operate on everyone, but even we like having a non-invasive option that is extremely safe and highly effective.
So, now you know tendonitis is an inflamed tendon and tendinosis is a degenerated tendon. I hope you also learned the importance of rest and proper treatment after even a minor injury. Early intervention helps keep your acute tendon injury from turning into tendonitis and your tendonitis into tendinosis. Tendinosis requires months to recover and sometimes surgery or High-energy Extracorporeal Shockwave Therapy. Both conditions are preventable. It is best to see your healthcare provider sooner rather than later to save yourself from months or years of pain and frustration if they do occur. Playing through the pain may not seem like a big deal now, but years from now, it may land you in an office like mine.
Dr. Ryan Sieg is a board-certified orthopedic surgeon specializing in sports medicine and osteoarthritis, as well as combat trauma having served in the Middle East. Dr. Sieg is a strong proponent that surgery should be the last resort, but that patients often lack any other option. Dr. Sieg has his BS in Biochemistry/Biophysics and MS in Organic Chemistry from the University of Oregon and his MD from the Uniformed Services University of Health Sciences.