Knee and Cartilage Rebuilding
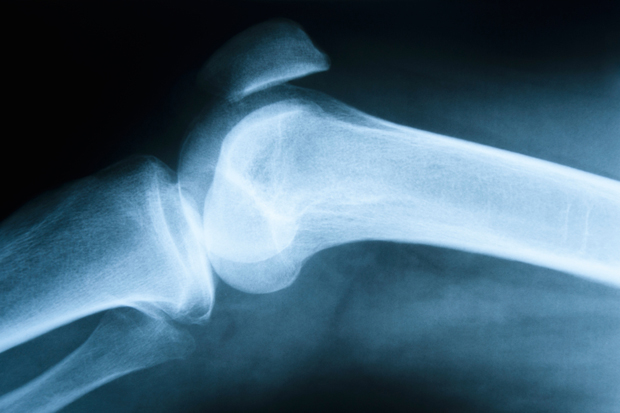
What treatments may be able to do for joint repair
Knee injuries are becoming increasingly common as society attempts to stay more active in order to achieve its goals of weight loss, stress reduction, general health and wellness, and athletic success. The push for a more active lifestyle has exploded as a result of society’s taking a greater interest in individual health and fears over what may happen with the future of health care. The drive to achieve athletic greatness is also more appealing than ever because of the desire for financial reward. The rampant trend toward joining CrossFit training facilities, boot camps, triathlon training groups, and running groups certainly is contributing to an increase in overuse injuries as we fight against the aging process. However, as bodies age, tendons, cartilage, and ligaments tend to lose some of their elasticity and water content, rendering them more prone to degenerative arthritis (roughening or thinning of joint cartilage), tendinosis (degeneration of a tendon), tendonitis (inflammation of a tendon), and partial or complete tears. In addition, bones tend to become softer, leading to more stress fractures.
Cartilage Injuries
When I see patients in my office who complain of joint pain, the most common cause is cartilage injuries. These injuries are usually due to a traumatic event, years of “wear and tear,” genetic inheritance, or congenital issues. Most commonly, cartilage becomes rough, frayed, and cracked, or it may simply become thinner. Finally, the cartilage separates. This can cause the cartilage to separate from the bone and becomes loose inside the joint. Symptoms of a cartilage problem include swelling during or after activity, catching, locking, popping, or instability. Pain may also occur while walking, during exercise, or simply while bending your knee. Some individuals, especially women, experience grinding or a “crunchy” sensation that suggests fairly advanced wear. If the wear is under the kneecap, then symptoms will occur while lunging, squatting, or climbing stairs. If the wear is on the weight-bearing surfaces, then the pain is usually worse while standing, walking, or running. Patients with cartilage damage often complain of achiness or stiffness, especially when sedentary, or they experience pain when the weather changes, especially when the barometric pressure drops.
Treatment of Cartilage Injuries
Initial treatment of a cartilage problem usually begins with avoidance of the aggravating activity, rest, ice, judicious use of an anti-inflammatory for one to two weeks, and/or a supportive brace or wrap. If these measures do not have a significant benefit, then you should see a physician to obtain X-rays and discuss an MRI. If the MRI confirms cartilage roughening, thinning, or a defect, then more invasive options such as injections or surgery may be appropriate.
Cortisone Injections
Cortisone has been a mainstay of treatment of joint issues for many years but should be used cautiously. It is appealing because of its rapid onset of action, usually within three to five days. The duration of its effect, however, is quite unpredictable, lasting as little as a week or as much as a year. Cortisone can be very helpful in reducing the irritability of a joint that is swollen and painful. There is concern regarding its use and the potential for causing the cartilage to break down further or weakening a ligament or tendon, such as in rotator cuff or Achilles tendon problems. Doctors usually avoid giving an injection directly into a tendon and limit cortisone injections to three per year. Cortisone may be used for treating bursitis, which is inflammation of the protective layer between a tendon and a bone or over bony prominences, such as elbows and knees.
PRP Injections
Platelet-rich plasma (PRP) injections are becoming increasingly common for the treatment of ligament injuries, tendon damage, and arthritic conditions. Common conditions that can be treated with PRP include the following: tennis elbow (lateral epicondylitis), golfer’s elbow (medial epicondylitis), plantar fasciitis, rotator cuff injuries, quadriceps tendinosis (degeneration or partial tearing), patellar tendinosis, collateral ligament sprains of the knee, and Achilles tendon injuries. The procedure is performed in the office setting and takes about 20 minutes. A sample of the patient’s own venous blood, usually from the elbow, is taken. A centrifuge device then isolates the platelet cells. While the cells are spinning, the area to be injected is numbed with a local anesthetic; after the injection, the site will be very painful for two to three days. Most patients usually have results within four to eight weeks and, while most require only a single injection, a second or third injection may be needed. PRP has been extensively studied and is felt to be safe with minimal side effects; I have helped many patients avoid surgery with this technique. How does it work? It is believed that the platelet cells release chemicals that attract other cells to the damaged area to start the inflammatory process and increase circulation to the area, the first phase of healing. PRP has been shown to decrease recovery time after ligament, tendon, and muscle injuries. It also is currently being utilized in the treatment of arthritic conditions by injecting the cells into a damaged joint. This procedure is not usually covered by insurance because it is still considered experimental by insurance companies. However, multiple published studies have demonstrated its efficacy and patients should feel safe if a doctor recommends this treatment. The cost can range from $500 to $1,000 per injection.
Stem Cell Injections
The latest and greatest in the treatment of orthopedic injuries is the use of your own stem cells to treat a variety of issues, including arthritis, cartilage defects, ligament tears, and tendon injuries. Until recently, stem cell treatments were allowed only in Europe. Because doctors use autologous stem cells (the patient’s own cells) from the pelvis, the controversy that is present with the use of embryonic or amniotic stem cells is avoided. These pelvic cells do decrease in number as we age, but the cells remain pluripotent, meaning that they can develop tissue that is similar or identical to the area in which they are injected or transplanted. The cells are harvested with a needle from the iliac crest, which is the top of the pelvis that is palpable just beneath the skin. While a local anesthetic can be used in the office, the procedure is less painful if performed in a surgical suite under moderate IV sedation. The cells are then injected into an arthritic or damaged joint, tendon, or ligament. The procedure takes about 20 to 30 minutes.
Alternatively, I have been using stem cells that can be transplanted during surgery into a cartilage defect in the knee or ankle. For this procedure, I use donor tissue in the form of a patch to cover the cartilage defect. Next, I suture the patch over the defect and seal the edges of the patch with fibrin glue (a medical grade super glue). The cells are then able to regenerate cartilage that resembles the original tissue.
Surgery
A variety of surgical options exist if the aforementioned conservative measures have failed. Physicians have the ability to debride (smooth) damaged cartilage, a process called a chondroplasty. We can also regenerate cartilage with a variety of techniques, including a microfracture procedure and an osteoarticular transfer system (OATS) procedure if the damaged area is small—that is, less than 1.5 cm. If the damaged area is larger than 1.5 cm, or if the person has failed prior surgery, then we will often use either donor cartilage, stem cells, or perform a Carticel procedure. A Carticel procedure is a two-stage procedure (aka an autologous chondrocyte implantation or ACI) that can be used to regenerate cartilage by using one’s own cartilage cells, which are harvested at the time of an arthroscopic surgery. The cartilage cells are then replicated in a laboratory and suspended in a gel, and the immature cartilage cells (chondrocytes) are injected beneath a patch to stimulate cartilage regeneration.
Consult Your Doctor
The good news is that there are treatment options for your aching joints. Depending on the severity of the problem, the choices available may have a variety of rehabilitation times and effectiveness. Talk to your doctor about which option would be best for your injury, but it is important to understand what each procedure entails.